Invasive measurement of physiological pressure, particularly arterial or intracardiac pressure, is a central component of critical care and anesthetic monitoring. These measurements provide real-time information about cardiovascular function and are essential for guiding treatment in unstable patients. The accuracy of such measurements depends not only on the placement of the catheter but also on the physical properties of the pressure transduction system [1].
There are two main methods for measuring pressure invasively. The first involves catheter-tip pressure sensors, which are miniature electronic devices placed directly at the site of interest. These sensors offer high precision and minimal signal distortion due to their location and the absence of intermediary components. However, they are expensive, prone to drift, and difficult to recalibrate once in place. The second method, more commonly used in clinical practice, relies on fluid-filled catheters connected to external pressure transducers. These systems are less costly and more versatile but are more susceptible to dynamic artifacts, especially from air bubbles, compliant tubing, and connector complexity [1, 2].
A key factor influencing the quality of the pressure signal is the system’s resonant frequency. Resonance occurs when the frequency of the physiological pressure waveform coincides with the natural frequency of the measuring system. This can cause overshooting and ringing in the recorded waveform, which leads to inaccurate interpretation of systolic and diastolic pressures. For this reason, it is important that the natural frequency of the system be well above the frequencies present in the physiological signal [2].
Closely related to resonance is the concept of damping. Damping refers to the dissipation of energy in the system and affects how the system responds to pressure changes. A system that is underdamped will overshoot and oscillate after a sudden pressure change, while an overdamped system will respond sluggishly and may miss important waveform features. The optimal damping factor has been shown to be approximately 0.7, where the pressure signal is faithfully transmitted without excessive oscillation or delay [1].
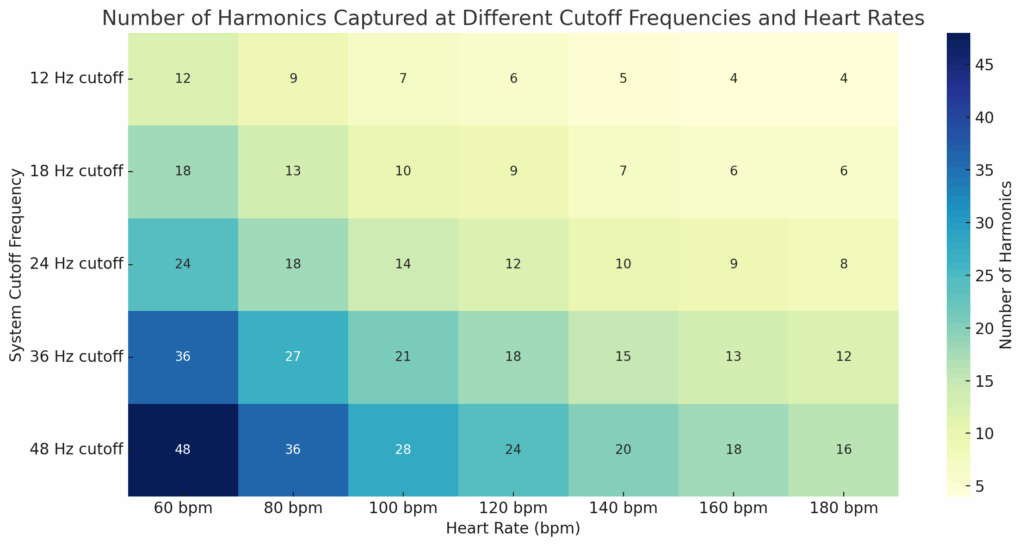
Another important aspect of pressure waveform fidelity is the ability of the system to transmit the higher-frequency components of the signal, known as harmonics. A pressure waveform, such as the arterial pressure curve, is composed of a fundamental frequency that corresponds to the heart rate and multiple harmonic frequencies that define the sharpness and detail of the waveform. To accurately reproduce the shape of this waveform, the system must capture at least the first eight to ten harmonics [1].
This requirement translates into a minimum frequency response or bandwidth. For a heart rate of 90 beats per minute, which corresponds to a fundamental frequency of approximately 1.5 Hz, the system must be able to accurately transmit frequencies up to at least 12 Hz. This ensures that the key harmonic components are preserved. For clinical systems intended to monitor heart rates up to 180 beats per minute, a bandwidth of 24 Hz or more is typically required [1].
To achieve this level of performance, certain design considerations are essential. Tubing should be short, stiff, and have a narrow bore to maximize the resonant frequency. The use of multiple stopcocks, connectors, or compliant components should be minimized to avoid excessive damping. The entire system must be carefully flushed with degassed fluid to remove air bubbles, which significantly lower the system’s natural frequency and introduce artifacts. Regular testing, such as the fast-flush test, should be used at the bedside to evaluate the dynamic behavior of the monitoring setup [1, 2].
In summary, the accuracy of invasive pressure measurements depends on both the catheter configuration and the physical characteristics of the measurement system. Resonance, damping, and frequency response all play a role in determining how faithfully the physiological pressure waveform is captured and displayed. A well-designed and correctly set up system will ensure that clinical decisions are based on reliable data.
References
- Stoker, M. R. (2004). Principles of pressure transducers, resonance, damping and frequency response. Anaesthesia and Intensive Care Medicine, 5(11), 371–375.
- Scruggs, V., Pietras, R. J., & Rosen, K. M. (1975). Frequency response of fluid-filled catheter-micromanometer systems used for measurement of left ventricular pressure. American Heart Journal, 89(5), 619–624.
