Measuring blood flow in the heart is essential for evaluating cardiac function and diagnosing various cardiovascular conditions. Several devices are employed for this purpose, each with its own methodology and application.
Thermodilution
One widely used technique for measuring cardiac output, which reflects blood flow from the heart, is thermodilution. This method involves the insertion of a catheter into a central vein, such as the jugular or femoral vein, which is then advanced into the right heart chambers, often reaching the pulmonary artery.
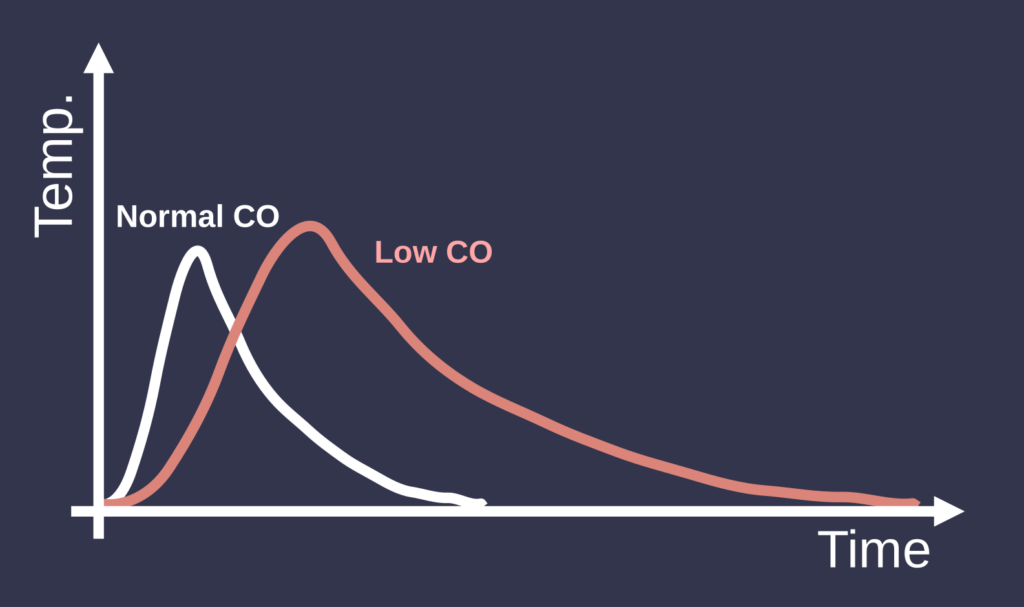
To measure blood flow, a known volume of cold saline is injected into the right atrium through the catheter. As the cold saline mixes with the blood, it lowers the blood temperature downstream. The catheter is equipped with a thermistor that continuously measures the blood temperature in the pulmonary artery. By analyzing the change in temperature over time, clinicians can calculate cardiac output using the Stewart-Hamilton equation, which takes into account the volume of saline injected, its temperature, and the resulting temperature change in the blood. This method is commonly utilized in critical care settings, particularly for monitoring cardiac output in patients with heart failure or those undergoing major surgery.
Echocardiography
Echocardiography is another vital technique, known for its non-invasive approach to visualizing the heart and assessing blood flow. In this method, the patient is positioned, typically on their left side, to optimize imaging. A transducer is placed on the chest, emitting high-frequency ultrasound waves that reflect off the heart structures.
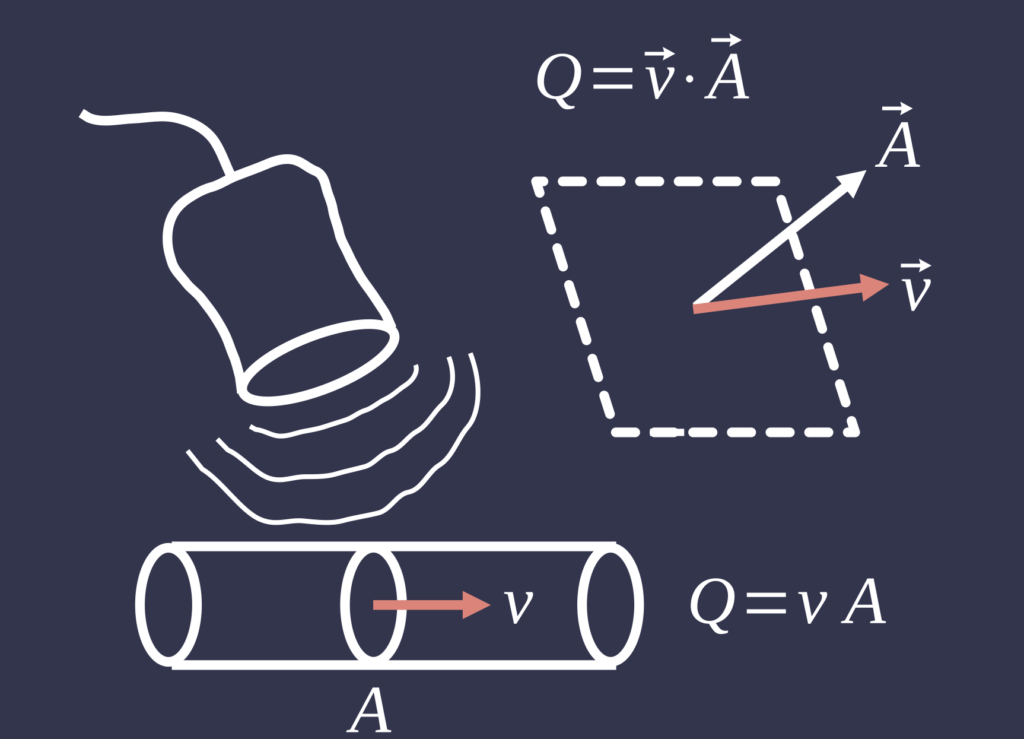
Using the Doppler technique, the device measures the velocity of blood flow across the heart valves and through the chambers. By obtaining blood flow velocities and the cross-sectional area of the heart chambers or valves, clinicians can calculate the volume flow rate using the continuity equation (Q = V × A), where Q is flow, V is velocity, and A is the area. This real-time imaging and flow data are displayed on a monitor, allowing for a comprehensive assessment of cardiac function. Echocardiography is widely available and invaluable for evaluating a range of cardiac conditions, including valve disease and heart failure.
Cardiovascular Magnetic Resonance Imaging (CMRI)
Cardiovascular magnetic resonance imaging (CMRI) is a technique that employs magnetic resonance imaging to provide detailed images of the heart and assess blood flow. In this procedure, the patient is positioned inside an MRI scanner, ensuring that any metallic objects are removed to prevent interference.
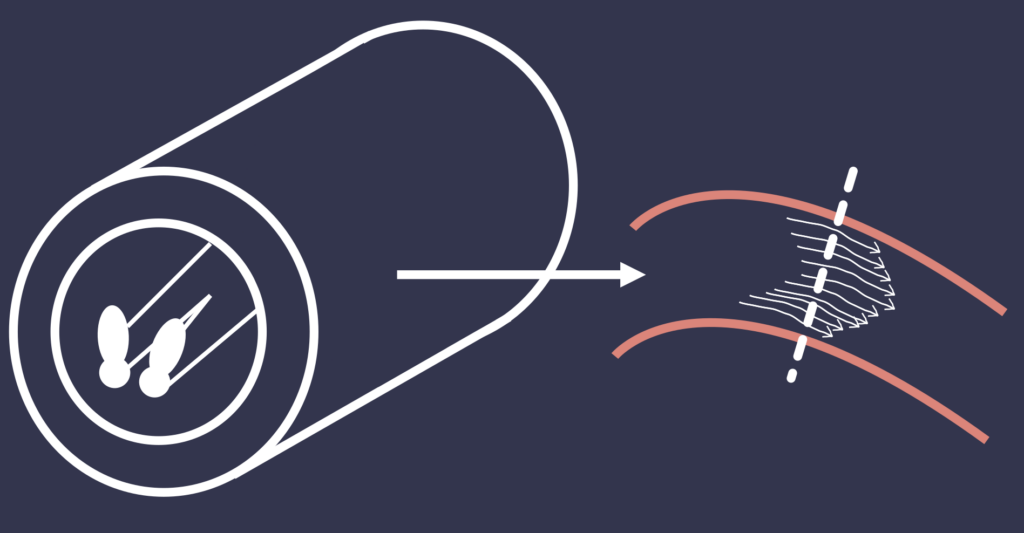
Sequences of images are captured while the heart is in various phases of the cardiac cycle, often with the use of a contrast agent to enhance blood flow visualization. CMRI utilizes velocity-encoded phase-contrast techniques to measure blood flow through specific areas of the heart, such as the left ventricle and major vessels. The resulting images are analyzed with specialized software to calculate flow rates based on velocity measurements and the cross-sectional area of the vessels. CMRI provides comprehensive information about cardiac anatomy and function, making it particularly useful for diagnosing congenital heart disease and cardiomyopathy.
Pulmonary Artery Flow Probe
The pulmonary artery flow probe offers a direct measurement of blood flow in the pulmonary artery. This method involves surgically implanting a flow probe around the pulmonary artery, which allows for continuous monitoring of blood flow. The probe utilizes electromagnetic or ultrasonic technology to measure blood flow as it passes through.
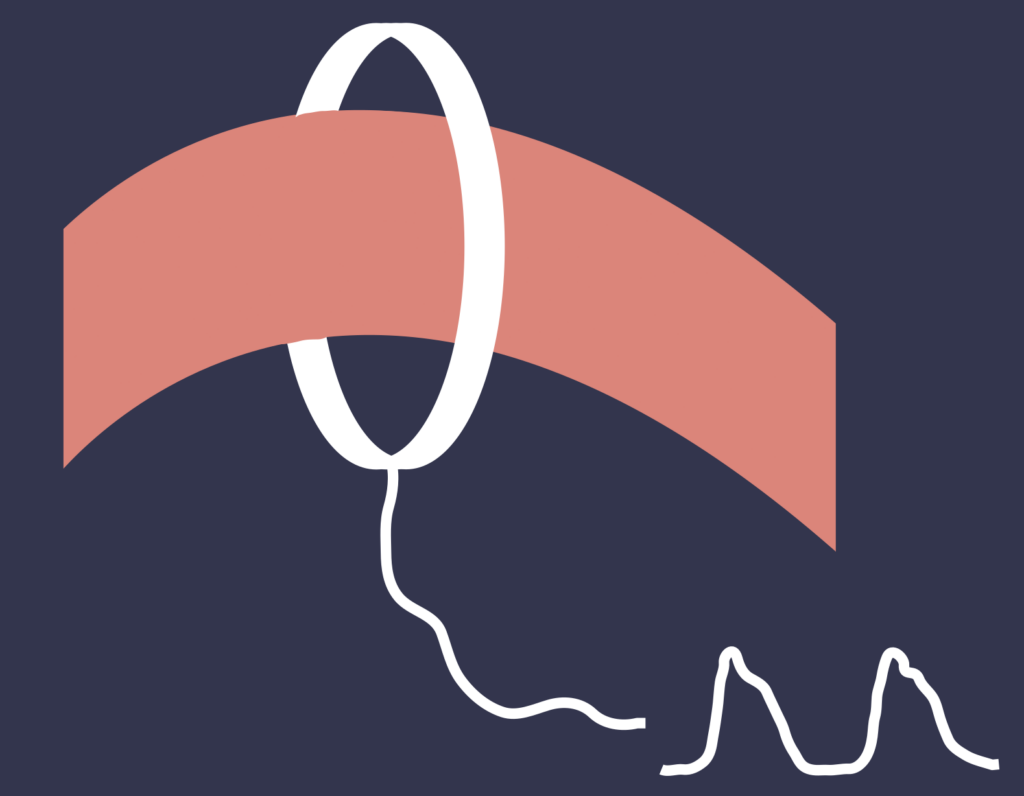
As blood moves through the probe, it generates an electrical signal proportional to the flow rate. This signal is then transmitted to a monitoring system that displays real-time blood flow data, allowing for continuous assessment. Regular calibration may be required to ensure the accuracy of the measurements. The pulmonary artery flow probe is particularly useful in research settings or specialized clinical environments, enabling real-time monitoring of pulmonary blood flow and providing valuable insights into heart function and pulmonary circulation.
Pulse contour analysis
The arterial pulse waveform is generated each time the heart contracts, sending blood through the arteries. By studying the shape of this pulse wave, doctors can gather important information about various aspects of cardiovascular health. For instance, the waveform can be used to estimate stroke volume, which is the amount of blood the heart pumps out with each beat. From this, the cardiac output—the total amount of blood the heart pumps per minute—can be calculated, providing a measure of overall heart function.

In practice, arterial pulse contour analysis is often used in critical care settings, such as intensive care units or during surgery, to monitor patients’ cardiovascular health in real time. The method can be performed in two main ways: invasive and non-invasive. The invasive approach involves inserting a catheter, usually in the radial artery, to continuously measure blood pressure, which is then analyzed to estimate key parameters like stroke volume. Non-invasive techniques, which use sensors on the wrist or fingers, offer a more comfortable alternative but are generally considered less precise than invasive methods.
